Understanding PCOS with Dr Jana Pittman: The questions you’re too afraid to Google
The acronym ‘PCOS’ (short for polycystic ovarian syndrome) gets thrown around regularly when someone has irregular periods, male pattern hair growth or infertility. But most of us don’t understand what it really means, or the fact that it is a ‘life-long’ condition.I am incredibly lucky to work under one of the leading doctors in reproductive medicine, Professor Bill Ledger, from the Royal Hospital for Women in Sydney, and a Professor of Obstetrics at the University of New South Wales. He has graciously agreed to triple-check my facts on all things PCOS.
What are the first signs of PCOS?
The signs and symptoms vary from person to person, but ovulatory dysfunction (which means irregular or infrequent periods), and hyperandrogenemia (higher testosterone levels that can cause hair growth or hair loss and acne) are commonly seen.On transvaginal ultrasound, multiple follicles (more than 20) are seen on at least one of the ovaries. It’s the most common endocrinopathy (hormone issue) in reproductive people.
Higher rates of mood disorders, eating disorders, psychosexual dysfunction and low self-esteem have also been reported.
Why does PCOS make your period come late or irregular?
The cause of PCOS is complex and multifactorial. Environmental influences, genetic factors and intrauterine variation can predispose a person to having PCOS. Essentially, at the peak of your reproductive life, the body creates several eggs each month called primordial follicles.They go through various stages of selection and atresia (die-off) due to sensitive hormone control until only one (or occasionally more) dominant follicle is released (ovulation).
In PCOS, the eggs get stuck at the ‘recruitment and selection’ stage and none become ‘dominant’ which means either irregular or no ovulation, and the diversion of steroidogenesis (hormone creation) towards testosterone pre-dominant. Hence lots of little follicles on the ultrasound, and the associated ‘androgen’ features of excessive hair growth and acne.
How is PCOS diagnosed?
In general, if you have menstrual cycles less than 21 days or more than 35 days, it is worth getting investigated.Your doctor will usually perform a blood test looking at your androgen levels (free and total testosterone), your follicle reserve (Anti-Müllerian hormone, AMH) and other things like an oral glucose tolerance test (for diabetes) and order an ultrasound scan. This is best using a transvaginal ultrasound probe but can be done with a transabdominal scan if a vaginal scan is not appropriate.
Can you get pregnant with PCOS?
Yes, however some people hoping to get pregnant will need help pre-conception with lifestyle changes like treating diabetes or reducing their weight. Then there are multiple treatment options from ovulation induction (medication to regulate the release of eggs) to IVF.Interestingly once pregnant, women with PCOS are at an increased risk of gestational diabetes and pre-eclampsia, so be sure to keep monitoring that with your doctor.
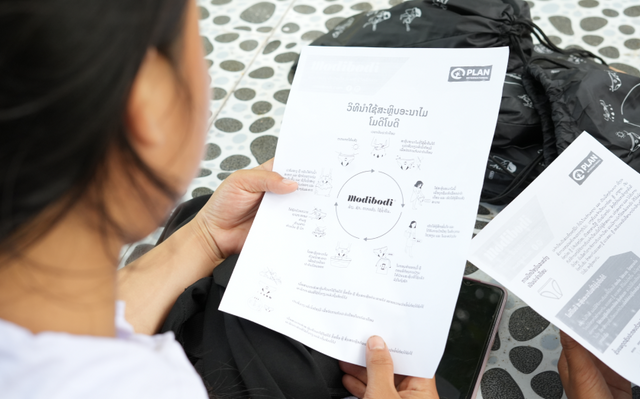
In terms of uniforms, as a Modibodi ambassador, I am happy that the PUMA x Modibodi period activewear range means we now have a solution that means the colour of our sports uniform is less problematic. But if it still bothers you, have a voice. Be brave and compete anyway but let your coach know you feel uncomfortable.”
Does PCOS affect your skin?
Acne is a real concern for many women with PCOS. As described above, the complex interplay of endocrine control means the androgen levels predispose women to skin breakouts.Here are some ways you can talk to your doctor about to help reduce acne caused by PCOS:
- Diabetes medication like metformin
- Changing your diet
- Increasing exercise to regulate insulin levels
- Using birth control
- Can PCOS make you feel depressed or affect your mood?
- Mood symptoms have been recognised as a concern for many women with PCOS. There is a particularly high prevalence of moderate to severe depression and anxiety disorders.
The cause of mood disturbances is thought to be associated with the pro-inflammatory state, insulin resistance, and elevated cortisol levels. There is also the consideration of body image around higher BMI, acne and hair growth that can cause some women psychological discomfort.
Are there any other important considerations with PCOS?
There are a few other things to think about when you have PCOS. One complication can be a higher risk of endometrial hyperplasia and cancer, especially if you also have a higher BMI.The overall risk remains low, so routine screening is not recommended but it's important to keep in mind, so you can consider preventative management like cycle regulation and progesterone therapy.
Interestingly, people with PCOS have higher rates of obstructive sleep apnoea compared to those without, independent of their BMI. All PCOS-sufferers need to be assessed for cardiovascular disease too as there has been an association with an increased risk for women with PCOS of hypertension, heart disease and stroke.
Now, I know this all sounds a little intense.
The key message here is that PCOS is more than just irregular periods and infertility. Awareness is key and many of these things are preventable, when you’re armed with the right advice.